By Laura Thornton
One of Kennedy Krieger Institute’s newest clinics is its Pediatric Post-COVID-19 Rehabilitation Clinic, which serves children and young adults up to age 21 experiencing lingering symptoms from COVID-19. Established in the summer of 2020, the clinic began seeing patients later that year. Since then, interest in the clinic has grown immensely, with clinic sessions recently increasing in frequency from once to twice a month.
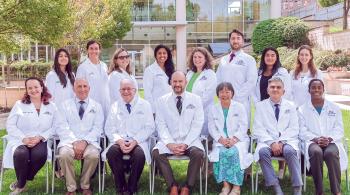
“Our clinic has expanded as needs have grown,” says pediatric neurologist Dr. Laura Malone, who co-directs the clinic with Dr. Amanda Morrow, a pediatric rehabilitation physician. In addition to Drs. Malone and Morrow, the clinic team includes physical therapists, a psychologist, neuropsychologists, a social worker, a nurse coordinator and an educational specialist.
“We follow a team-based approach, and create a cohesive and holistic rehabilitation plan for each patient,” Dr. Malone says.
“Having different providers with different perspectives gives patients and families the opportunity to express the multiple ways in which they’ve been affected, including physically, cognitively and emotionally, by COVID-19,” adds Bridget Fulford, the clinic’s social worker.
In-Depth Evaluation
Symptoms of long COVID-19 include fatigue, brain fog, dizziness, headaches, anxiety and depression, and can last for months. It’s a relatively new illness, but the clinic team has plenty of experience to go on. “We’ve learned a lot based on what our patients and other clinicians are describing,” Dr. Morrow says. “And we’re able to bring in treatment strategies that we use for patients with well-studied diagnoses” like concussion, chronic fatigue syndrome and postural orthostatic tachycardia syndrome (POTS).
“There’s a lot of cross-over between concussion and long COVID-19 in terms of recommendations,” adds registered nurse Sherri Clark, the clinic’s coordinator. “The piece that’s different is that we don’t know how long it will take to get better.”
Over the past year, the team has evaluated about 50 patients. During an evaluation, which usually lasts about four hours, the patient and their parents or guardians meet with each clinic team member. “We focus a lot on patient functioning—how well they’re able to do daily tasks, tolerate physical activity and participate in school and extracurricular activities—as well as on their overall social-emotional well-being,” Dr. Morrow says.
Next, team members gather to discuss their observations and compile a set of recommendations. Any patients experiencing brain fog or difficulties with attention or concentration—more than half of the clinic’s patients—are referred for neuropsychological assessment.
“Recommendations and follow-up are very individualized,” Dr. Malone says. “Occasionally we’ll recommend medication, but we focus on lifestyle modifications, exercise and physical therapy, and when needed, seeing mental health providers. But we also complete diagnostic work-ups to rule out other conditions that might be mimicking some of the symptoms of long COVID-19.”
For patients visiting Kennedy Krieger from far away, “We’ll provide as much guidance as possible for finding the right people to partner with locally,” she adds. Baltimore-area patients often receive care through the Institute’s outpatient clinics (such as its Physical Therapy Clinic) or Specialized Transition Program, a neurorehabilitation day hospital, to receive weekly-to-daily physical, occupational, speech and behavioral health therapies.
Families usually return for a follow-up appointment three to six months later. “And they’re always welcome to reach out to us in the meantime with any questions or concerns,” Clark says.
‘We’re Here to Help’
Long COVID-19 often impacts patients’ mental health, and children and teens are no exception. Clinic psychologist Dr. Ellen Henning screens patients for anxiety and depression, which can be impacted by the disease, and connects them with resources and interventions—such as cognitive behavioral therapy—that can help.
“Some of our patients are high-achieving students who can’t remember complex math equations anymore, and no longer feel confident in themselves,” Fulford says. “We’ve seen a lot of kids with severe anxiety and depression because they’re not able to have a regular school day or see friends. It’s impacted their whole life—and their whole family. I look at all the stressors and barriers they’re facing, and provide recommendations—as well as comfort and validation.”
“The fatigue the kids are experiencing is really difficult for outsiders to understand,” and many patients’ parents have long COVID-19, too, Clark says.
“Some patients and families say this is the first time anyone has believed their symptoms,” Fulford adds, “and the first time they’ve been able to get help.”
The clinic is working with Kennedy Krieger’s Specialized Health Needs Interagency Collaboration (SHNIC), directed by Dr. Joan Carney, assistant vice president of clinical programs. Funded by the Maryland State Department of Education, SHNIC is staffed by nurse educators and education specialists who work with schools across Maryland—free of charge—to help facilitate the inclusion of students with special health needs, including those with long COVID-19, in the classroom. SHNIC nurse educators conduct training sessions for school health supervisors and student services directors as well as home and hospital educators, and offer case-by-case consultations to support student success in the classroom.
The clinic is part of national and international research studies to learn more about the effects of long COVID-19 on children. “We’re hoping to better define the symptoms, and better understand the course of the illness and what treatments are best,” Dr. Morrow explains.
In the meantime, the clinic’s patient list is growing. “We are dedicated to making sure families are heard, and that we can give them next steps to promote comfort and functioning,” Dr. Henning says. “Feedback is often, ‘Wow, this is really helpful.’”
"Validation goes a long way, especially for families who’ve been told that these symptoms aren’t real.” – Bridget Fulford, social worker
“The greatest thing I’ve learned while working in this clinic is that validation goes a long way, especially for families who’ve been told that these symptoms aren’t real,” Fulford says. “But these symptoms are absolutely real. We’re here to help, and we won’t dismiss what you’re saying.”