Combatting the Lack of Implicit Bias Training in Medical Education
Authors: Hanna Leonard; and Alyssa Thorn, Esq.; Mallory Finn, Esq.
Background: Implicit Bias in the Clinical Field
When implicit bias is neither recognized nor managed in medical education, it can negatively impact—to a significant extent—medical students’ future success in the field, as well as the health and well-being of the students’ future patients and patient families.
In the clinical realm, implicit bias refers to physicians and medical students automatically stereotyping patients on the basis of race, gender, weight and disability, among other factors. Research shows that medical students are not extensively taught to recognize their own forms of implicit bias when diagnosing a patient and communicating with the patient’s family. When implicit bias occurs while diagnosing a patient with a developmental disability, and the bias is not discovered and managed, the negative impacts can be far-reaching.
Failure to Address Implicit Bias in Medical Education
In general, the effects of implicit biases in healthcare are understudied and can be difficult to evaluate using the existing tools, which have been created and utilized within the contexts of other professions. Data reflect that physicians and nurses manifest implicit biases to a similar degree as does the general population. However, the problem with implicit biases in healthcare, specifically, is that they influence the decisions made by healthcare professionals without their knowledge and despite their best intentions.
When these biases are not recognized and managed, the following characteristics of patients can potentially act as determinant factors in their care: race/ethnicity, gender, socio-economic status, age, mental illness, weight, disability and, for patients with brain injuries, the belief that the patients have contributed to their injuries. These biases can lead to the continuation of healthcare disparities by shaping behavior and by producing differences in medical treatment. Additionally, these biases operate to the disadvantage of the patient, who is typically in a vulnerable position.
Negative Impacts on Physician-Patient Relationships and Treatment Plans
Implicit bias, when expressed in the process of diagnosis, can negatively impact physician-patient interactions, change treatment plans, and perpetuate the already existing disparities in the healthcare system.
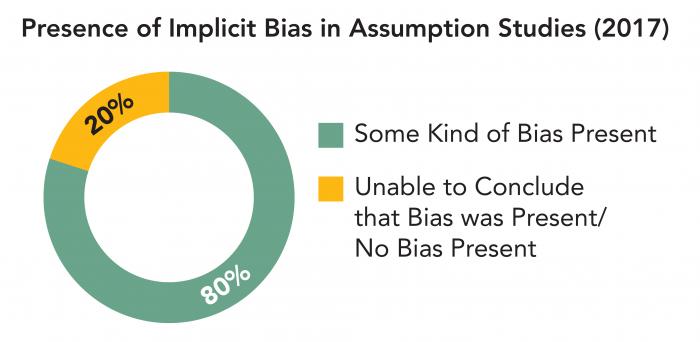
In certain cases, research has concluded that there is a significant correlation between the level of implicit bias held by a clinician and the quality of care that clinician provides. In 20 out of 25 assumption studies, it was found that some kind of bias against the patient under examination was evident in the diagnosis, treatment recommendations, number of questions asked of the patient, number of tests ordered, or other action by the clinician.
Potential Solutions
One potential solution is to diversify the student body at medical schools. Data has found that Black doctors possess little to no implicit biases concerning race while White doctors expressed an explicit preference for white male patients (Sabin et. al. 2012). Hispanic female doctors did not show a racial preference for patients, neither implicit nor explicit, but Hispanic male doctors showed a strong preference for white male patients (Sabin et. al. 2012). Perhaps if medical school classes were more diverse in terms of race and ethnicity, implicit biases could be minimized more organically. However, diversifying medical school classes can be used in tandem with introducing educational means to combat implicit biases in healthcare.
Another solution is to create a class focused solely on reducing implicit biases, and to require medical students to take this class for the duration of their time in medical school. These classes are most effective as discussion-based, small-group classes; this is the best way for students to feel comfortable sharing their reflections concerning patients. This class must consist of implicit bias testing throughout the time that the students are enrolled so that implicit biases can be tracked, and their minimization and management can be recorded for the student to reference.
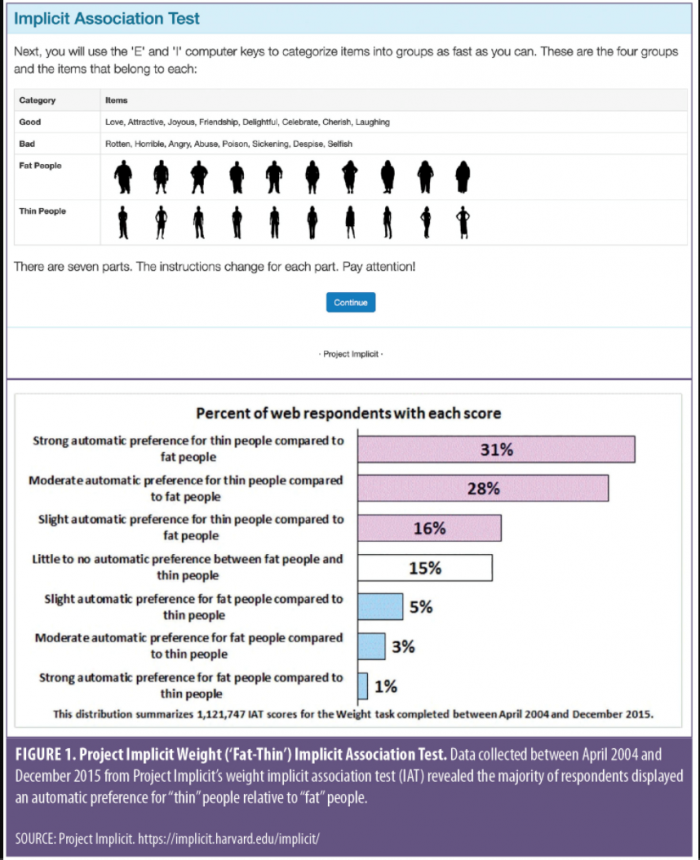
The best testing mechanism to do so is the Implicit Association Test (IAT), which measures implicit biases by tracking the amount of time it takes for a participant to match a social group (e.g., a group of people with disabilities or obesity), with a characteristic (e.g., good or stubborn). Implicit bias becomes operationalized when test-takers take a shorter amount of time to match a characteristic to a social group because they already have that association developed. Once implicit biases are identified, the professor will then teach the students about identifying, managing and minimizing those implicit biases.
In sum, medical schools can make great strides toward diminishing disparities within healthcare by diversifying their student bodies and requiring their students to take classes about implicit bias.
Further Research
Further research needs to be conducted within this field. Unfortunately, there is not as much data as there should be regarding the prevalence of implicit bias in medicine. Specifically, more data is needed about the correlational effects of implicit biases and poor healthcare decisions and outcomes. Additionally, studies need to be conducted on the different methods of implicit bias training. Data from these studies will guide medical education programs toward investing in the most effective methods.
References
Chapman, E., Kaatz, A., & Carnes, M. (November 2013). Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. Journal of General Internal Medicine, 28(11), 504–510. Retrieved from https://pubmed.ncbi.nlm.nih.gov/23576243/
Eadie, T., Sroka, A., Wright, A., & Merati, A. (July 2011). Does knowledge of medical diagnosis bias auditory-perceptual judgments of dysphonia? Journal of Voice, 25(4), 420–429. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20347262/
FitzGerald, C., & Hurst, S. (March 1, 2017). Implicit bias in healthcare professionals: a systematic review. BMC Medical Ethics, 18(1), 19. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28249596/
Gonzalez, C., Kim, M., & Marantz, P. (2014). Implicit bias and its relation to health disparities: a teaching program and survey of medical students. Teaching and Learning in Medicine, 26(1), 64– 71. Retrieved from https://pubmed.ncbi.nlm.nih.gov/24405348/
Sabin, Dr. Janice, Nosek, Dr. B., Greenwald, Dr. A., & Rivara, Dr. F. Physicians’ Implicit and Explicit Attitudes About Race by MD Race, Ethicity, and Gender. Journal of Healthcare for the Poor and Underserved, 20(3), 896-913. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3320738/
Sukhera, J., Watling, C., & Gonzalez, C. (May 2020). Implicit Bias in Health Professions: From Recognition to Transformation. Academic Medicine, 95(5), 717–723. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31977339/
Teal, C., Shada, R., Gill, A., Thompson. B., et al. (May 2010). When best intentions aren’t enough: helping medical students develop strategies for managing bias about patients. Journal of General Internal Medicine, 25(Suppl. 2), S115–S118. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20352504/
